Blog

November 17, 2025
Do you ever feel anxious, irritable and overwhelmed in the run up to your period? Do you think it's hard to control your temper and feel just not like yourself? These are common signs of premenstrual syndrome (PMS) which is a term used to describe a number of physical and emotional symptoms you may experience in the run up to your period. The exact cause is not clearly understood but it is thought to be due to a change in your hormone levels in the second half of your cycle. Notably a rapid fall in the level of progesterone, (our soothing, calming, and relaxing hormone), could very well be at play. For some women, the first time they really begin to notice symptoms of PMS is as they enter the perimenopause as their natural hormones, and in particular, their progesterone levels begin to fall. For others, as they hit perimenopause, their lifelong PMS symptoms become more intense and start to appear earlier and earlier in their cycle. It is really important to acknowledge the enormous impact that these symptoms can have on a woman’s life and the impact they can have on those around them at home and in the workplace. So what can we do about it? In all cases, whether perimenopausal or not, following a healthy diet that focuses on maintaining a well-balanced blood sugar is vital. Regular exercise, minimising alcohol intake and getting sufficient sleep as well as taking supplements such as magnesium and B vitamins will also help. If anxiety is a major factor then a daily supplement of Ashwagandha can be very beneficial. For moderate PMS, supplementary progesterone therapy in the second half of the cycle can be extremely beneficial. In some cases, overriding the body’s natural cycle with a body-identical combined contraceptive pill such as Zoely, taken with no breaks brings relief. In other cases, hormone replacement therapy involving natural oestrogen and progesterone is used. Whether PMS has always been a part of your life and you’d like to take back control, or if you have developed cyclical mood changes more recently and want to understand what is happening and how to tackle it, our specialist clinicians are ready to listen. We are able to help you find the right strategy whatever your stage of life.
November 17, 2025
On World Mental Health Day we want to draw your attention to the critical role that your hormones play in your mental health. The hormonal changes we experience during the perimenopause and menopause can have a profound effect on our mental health, with depression, anxiety, mood swings, and loss of self-esteem and confidence being extremely common. Women commonly describe losing their sense of self and this can have a significant impact on their relationships both at work and at home. Fluctuations in hormone levels including oestrogen, progesterone, and testosterone can have a direct effect on our mood. In particular, progesterone is an anti-anxiety hormone that is important for sleep, whilst testosterone is known to elevate the mood and boost stamina. We must also not underestimate the effects that changes in body shape, fertility and the quality of sleep can have on our mood and self-esteem. Regulating hormone levels during this time with hormone replacement therapy is a very effective way to tackle the mental health issues associated with this time in a woman’s life and can be far more effective than traditional antidepressant medications. Lifestyle interventions such as exercise, dietary changes, and reducing alcohol intake are also very important. Above all it is important to remember you are not alone and there is help available either via your GP, a specialist hormone clinic , or via support charities such as the Samaritans.

November 17, 2025
There are multiple approaches to HRT (Hormone Replacement Therapy), the medicine-based process for relieving symptoms of menopause. In this short guide, we look at the effectiveness, benefits, and risks of transdermal oestrogens. What are transdermal oestrogens? Transdermal oestrogens are applied directly to your skin as using either patches, gels, or sprays. Replacing oestrogen helps in manage the majority of menopausal symptoms. Oestrogen has also been shown to be effective in maintaining or increasing bone mineral density . When HRT is taken within 10 years of menopause or below the age of 60 it can reduce the risk of cardiovascular disease. The advantage of transdermal delivery is that it allows oestrogen to enter your bloodstream directly, avoiding your liver, which reduces the risk of blood clots (VTE) or stroke seen with oral forms. Who is the transdermal method best suited to? Transdermal HRT is particularly suited for women who want to take HRT for their menopausal symptoms but have a history of, or risk of blood clots, liver disease, migraines or are deemed higher risk for cardiovascular disease or stroke. It’s also a good option for those who would benefit from a non-oral method of medication due to gastrointestinal disease or a history of gastric bypass surgery. Additionally, it can benefit women who seek a steady release of hormones without the peaks and troughs that sometimes occur with oral HRT. What is venous thromboembolism (VTE)? Venous thromboembolism ( VTE ) is a serious condition where blood clots form in the deep veins, primarily in the legs (known as deep vein thrombosis, or DVT). These clots can dislodge and travel through the bloodstream to the lungs, causing a potentially life-threatening blockage called a pulmonary embolism (PE). VTE can result from various factors, including prolonged immobility such as long-haul flights, certain medical conditions, surgery, or a genetic predisposition to clotting. Is transdermal HRT more suitable for people at risk of VTE? Yes, transdermal HRT is generally considered more suitable for individuals at risk of VTE. Unlike oral HRT, transdermal HRT delivers hormones directly into the bloodstream through the skin, bypassing the liver. This method reduces the impact on clotting factors and liver metabolism, leading to a lower risk of developing blood clots compared to oral oestrogen. Therefore, for those with a history or heightened risk of VTE, transdermal HRT is the preferred choice. Which type of transdermal HRT is most effective? The effectiveness of transdermal HRT – whether in the form of patches, gels, or sprays – is generally considered similar across the different delivery methods. The choice between them depends on personal preference, lifestyle, skin sensitivity, and ease of use. Patches – Provide a steady release of hormones and are changed once or twice a week. They are convenient but can cause skin irritation for some users. Gels – Applied daily, allowing for more flexibility in dosing. They’re less likely to cause skin irritation but require careful application and takes time to absorb before you can get dressed. Sprays – Also applied daily, they are a newer option and can be an alternative for those who have skin reactions to patches or issues with gels. Ultimately, the “most effective” type is the one that best aligns with your personal preference and in consultation with a healthcare professional. Are there any risks in using transdermal oestrogens? Yes, like all forms of HRT, transdermal oestrogens do carry some risks, although they might be lower in certain aspects compared to oral oestrogens. The key risks include: Hormone-sensitive cancers – Use of oestrogens has been linked to an increased risk of certain hormone-sensitive cancers , notably breast cancer. Be sure to discuss personal and family cancer histories with a hormone specialist before starting treatment. Skin reactions – Some individuals may experience skin irritation or allergic reactions at the site of application, particularly with patches. Endometrial hyperplasia and cancer – In women with an intact uterus, oestrogen therapy can increase the risk of endometrial hyperplasia and cancer so progesterone must also be added to protect the lining of the uterus. Other side effects – These can include breast tenderness, nausea, headaches, and mood changes, although they may be less severe than with oral oestrogens. Regular monitoring and appropriate screenings are important during the course of your treatment, to minimise the risk of any serious complications. It is important to keep up to date with routine health screenings such as mammograms and cervical smears and to perform regular breast self-examination. Need help regaining your hormone balance? Hormone imbalance can occur at any time during a woman’s life. We understand the impact these symptoms can have on you, your family, your work, and your relationships. We offer advice, support, and treatment to get you back to feeling you again. Book a video consultation with us today or speak to our practice manager for further details.
November 17, 2025
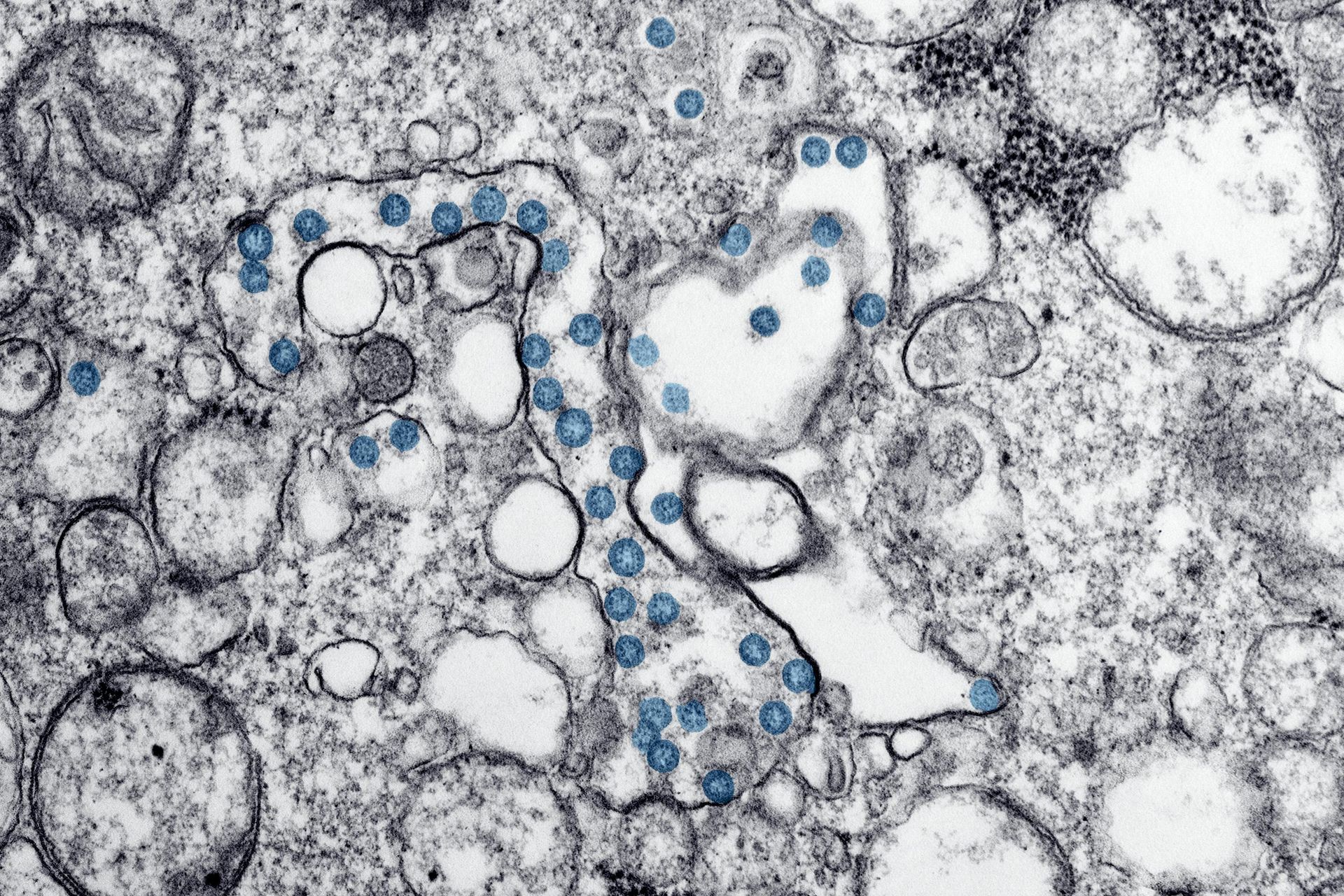
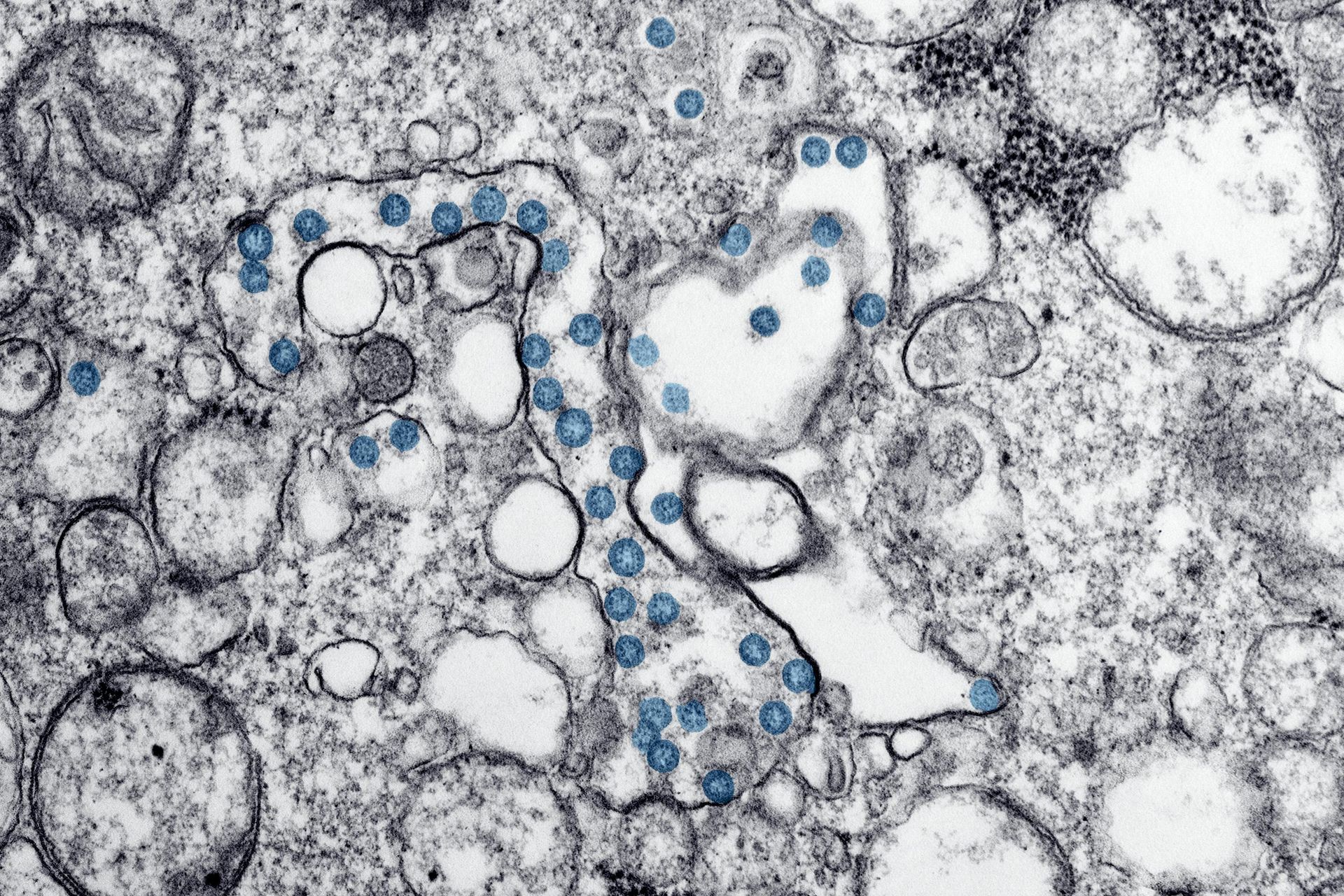
Recent research is shedding light on the significant role of the gut microbiome in our overall health and susceptibility to various illnesses. The gut microbiome, a complex community of microorganisms residing in our digestive tract, has been linked to numerous bodily functions and health outcomes. As scientists delve deeper into this area, the potential for groundbreaking discoveries continues to grow. One area of interest is the effect of fermented foods on the immune system. Fermented foods, rich in beneficial microbes, not only stimulate the immune system but also support the growth of other beneficial microorganisms in our gut. Among these foods, kombucha—a fermented tea—has gained popularity for its numerous health benefits. Research indicates that regular consumption of kombucha can significantly reduce oxidative stress and inflammation, enhance the liver detoxification process, and improve gut health by addressing intestinal dysbiosis, an imbalance in gut bacteria. These findings highlight the potential of kombucha as a natural, health-promoting beverage. Furthermore, we are beginning to understand how the gut microbiome influences hormone metabolism. This is particularly relevant for women undergoing menopause, a phase marked by hormonal fluctuations. Recognising the importance of gut health during this transition, we are thrilled to partner with a local company, @ holoskombucha , to provide our workshop attendees with a selection of delicious, organic kombucha drinks. Our collaboration with Holos Kombucha allows us to offer our attendees not only a tasty beverage but also a means to support their gut health during the menopause transition. As we continue to explore the profound impact of the gut microbiome on health, we look forward to deepening this partnership and discovering more ways to enhance wellness through natural, fermented foods. https://holoskombucha.com/collections/shop-now

November 17, 2025
Do you ever feel anxious, irritable and overwhelmed in the run up to your period? Do you think it's hard to control your temper and feel just not like yourself? These are common signs of premenstrual syndrome (PMS) which is a term used to describe a number of physical and emotional symptoms you may experience in the run up to your period. The exact cause is not clearly understood but it is thought to be due to a change in your hormone levels in the second half of your cycle. Notably a rapid fall in the level of progesterone, (our soothing, calming, and relaxing hormone), could very well be at play. For some women, the first time they really begin to notice symptoms of PMS is as they enter the perimenopause as their natural hormones, and in particular, their progesterone levels begin to fall. For others, as they hit perimenopause, their lifelong PMS symptoms become more intense and start to appear earlier and earlier in their cycle. It is really important to acknowledge the enormous impact that these symptoms can have on a woman’s life and the impact they can have on those around them at home and in the workplace. So what can we do about it? In all cases, whether perimenopausal or not, following a healthy diet that focuses on maintaining a well-balanced blood sugar is vital. Regular exercise, minimising alcohol intake and getting sufficient sleep as well as taking supplements such as magnesium and B vitamins will also help. If anxiety is a major factor then a daily supplement of Ashwagandha can be very beneficial. For moderate PMS, supplementary progesterone therapy in the second half of the cycle can be extremely beneficial. In some cases, overriding the body’s natural cycle with a body-identical combined contraceptive pill such as Zoely, taken with no breaks brings relief. In other cases, hormone replacement therapy involving natural oestrogen and progesterone is used. Whether PMS has always been a part of your life and you’d like to take back control, or if you have developed cyclical mood changes more recently and want to understand what is happening and how to tackle it, our specialist clinicians are ready to listen. We are able to help you find the right strategy whatever your stage of life.
November 17, 2025
On World Mental Health Day we want to draw your attention to the critical role that your hormones play in your mental health. The hormonal changes we experience during the perimenopause and menopause can have a profound effect on our mental health, with depression, anxiety, mood swings, and loss of self-esteem and confidence being extremely common. Women commonly describe losing their sense of self and this can have a significant impact on their relationships both at work and at home. Fluctuations in hormone levels including oestrogen, progesterone, and testosterone can have a direct effect on our mood. In particular, progesterone is an anti-anxiety hormone that is important for sleep, whilst testosterone is known to elevate the mood and boost stamina. We must also not underestimate the effects that changes in body shape, fertility and the quality of sleep can have on our mood and self-esteem. Regulating hormone levels during this time with hormone replacement therapy is a very effective way to tackle the mental health issues associated with this time in a woman’s life and can be far more effective than traditional antidepressant medications. Lifestyle interventions such as exercise, dietary changes, and reducing alcohol intake are also very important. Above all it is important to remember you are not alone and there is help available either via your GP, a specialist hormone clinic , or via support charities such as the Samaritans.

November 17, 2025
There are multiple approaches to HRT (Hormone Replacement Therapy), the medicine-based process for relieving symptoms of menopause. In this short guide, we look at the effectiveness, benefits, and risks of transdermal oestrogens. What are transdermal oestrogens? Transdermal oestrogens are applied directly to your skin as using either patches, gels, or sprays. Replacing oestrogen helps in manage the majority of menopausal symptoms. Oestrogen has also been shown to be effective in maintaining or increasing bone mineral density . When HRT is taken within 10 years of menopause or below the age of 60 it can reduce the risk of cardiovascular disease. The advantage of transdermal delivery is that it allows oestrogen to enter your bloodstream directly, avoiding your liver, which reduces the risk of blood clots (VTE) or stroke seen with oral forms. Who is the transdermal method best suited to? Transdermal HRT is particularly suited for women who want to take HRT for their menopausal symptoms but have a history of, or risk of blood clots, liver disease, migraines or are deemed higher risk for cardiovascular disease or stroke. It’s also a good option for those who would benefit from a non-oral method of medication due to gastrointestinal disease or a history of gastric bypass surgery. Additionally, it can benefit women who seek a steady release of hormones without the peaks and troughs that sometimes occur with oral HRT. What is venous thromboembolism (VTE)? Venous thromboembolism ( VTE ) is a serious condition where blood clots form in the deep veins, primarily in the legs (known as deep vein thrombosis, or DVT). These clots can dislodge and travel through the bloodstream to the lungs, causing a potentially life-threatening blockage called a pulmonary embolism (PE). VTE can result from various factors, including prolonged immobility such as long-haul flights, certain medical conditions, surgery, or a genetic predisposition to clotting. Is transdermal HRT more suitable for people at risk of VTE? Yes, transdermal HRT is generally considered more suitable for individuals at risk of VTE. Unlike oral HRT, transdermal HRT delivers hormones directly into the bloodstream through the skin, bypassing the liver. This method reduces the impact on clotting factors and liver metabolism, leading to a lower risk of developing blood clots compared to oral oestrogen. Therefore, for those with a history or heightened risk of VTE, transdermal HRT is the preferred choice. Which type of transdermal HRT is most effective? The effectiveness of transdermal HRT – whether in the form of patches, gels, or sprays – is generally considered similar across the different delivery methods. The choice between them depends on personal preference, lifestyle, skin sensitivity, and ease of use. Patches – Provide a steady release of hormones and are changed once or twice a week. They are convenient but can cause skin irritation for some users. Gels – Applied daily, allowing for more flexibility in dosing. They’re less likely to cause skin irritation but require careful application and takes time to absorb before you can get dressed. Sprays – Also applied daily, they are a newer option and can be an alternative for those who have skin reactions to patches or issues with gels. Ultimately, the “most effective” type is the one that best aligns with your personal preference and in consultation with a healthcare professional. Are there any risks in using transdermal oestrogens? Yes, like all forms of HRT, transdermal oestrogens do carry some risks, although they might be lower in certain aspects compared to oral oestrogens. The key risks include: Hormone-sensitive cancers – Use of oestrogens has been linked to an increased risk of certain hormone-sensitive cancers , notably breast cancer. Be sure to discuss personal and family cancer histories with a hormone specialist before starting treatment. Skin reactions – Some individuals may experience skin irritation or allergic reactions at the site of application, particularly with patches. Endometrial hyperplasia and cancer – In women with an intact uterus, oestrogen therapy can increase the risk of endometrial hyperplasia and cancer so progesterone must also be added to protect the lining of the uterus. Other side effects – These can include breast tenderness, nausea, headaches, and mood changes, although they may be less severe than with oral oestrogens. Regular monitoring and appropriate screenings are important during the course of your treatment, to minimise the risk of any serious complications. It is important to keep up to date with routine health screenings such as mammograms and cervical smears and to perform regular breast self-examination. Need help regaining your hormone balance? Hormone imbalance can occur at any time during a woman’s life. We understand the impact these symptoms can have on you, your family, your work, and your relationships. We offer advice, support, and treatment to get you back to feeling you again. Book a video consultation with us today or speak to our practice manager for further details.
November 17, 2025
Recent research is shedding light on the significant role of the gut microbiome in our overall health and susceptibility to various illnesses. The gut microbiome, a complex community of microorganisms residing in our digestive tract, has been linked to numerous bodily functions and health outcomes. As scientists delve deeper into this area, the potential for groundbreaking discoveries continues to grow. One area of interest is the effect of fermented foods on the immune system. Fermented foods, rich in beneficial microbes, not only stimulate the immune system but also support the growth of other beneficial microorganisms in our gut. Among these foods, kombucha—a fermented tea—has gained popularity for its numerous health benefits. Research indicates that regular consumption of kombucha can significantly reduce oxidative stress and inflammation, enhance the liver detoxification process, and improve gut health by addressing intestinal dysbiosis, an imbalance in gut bacteria. These findings highlight the potential of kombucha as a natural, health-promoting beverage. Furthermore, we are beginning to understand how the gut microbiome influences hormone metabolism. This is particularly relevant for women undergoing menopause, a phase marked by hormonal fluctuations. Recognising the importance of gut health during this transition, we are thrilled to partner with a local company, @ holoskombucha , to provide our workshop attendees with a selection of delicious, organic kombucha drinks. Our collaboration with Holos Kombucha allows us to offer our attendees not only a tasty beverage but also a means to support their gut health during the menopause transition. As we continue to explore the profound impact of the gut microbiome on health, we look forward to deepening this partnership and discovering more ways to enhance wellness through natural, fermented foods. https://holoskombucha.com/collections/shop-now
Symptom Checklist
For this project, the challenge was in rebranding an established product to attract new audiences, while ensuring that current users feel connected. The results were outstanding.
Hormones
For this project, the challenge was in rebranding an established product to attract new audiences, while ensuring that current users feel connected. The results were outstanding.